Aesthetic restorative masterclass: pressure formed composites

Published on 05/01/2023
By Ahmed Tadfi
Ahmed Tadfi describes the use of minimally invasive pressure formed composite techniques for the aesthetic restoration of multiple maxillary anterior and premolar teeth in a single appointment.
Direct composite is increasingly considered to be the treatment of choice for rehabilitation of the worn dentition.1,2 Additive techniques that bond composite to no-prep or minimally invasive tooth preparations present irrefutable advantages over indirect restorations, which are prone to catastrophic failure.1,2
Evidence has been growing since the late 1990s that composite can be used for the long-term management of tooth wear in all age groups,1 and that the most common modes of failure (chipping, wear, marginal stain) are easily treated by repolishing, refurbishment or repair techniques, rather than total restoration replacement.1
However, the freehand placement of multiple direct composite restorations is inherently challenging regarding occlusal/aesthetic control and appointment duration.1
As a result, there has been recent renewed interest in injection and pressure formed techniques that enable clinicians to replicate pre-approved functional and aesthetic prescriptions efficiently and predictably using:
A pre-operative wax-up (traditional or digital)
A translucent silicone template (constructed at chairside or in a laboratory)
Highly filled composite resins (often heated or flowable to enhance adaptation/flow)
Tooth separators e.g. PTFE tape or metal separators (SmileFast™)
While injection/ pressure formed procedures still have a significant learning curve, and are not suited to polychromatic techniques, mastery offers a range of potential advantages.
The following complex clinical case demonstrates the use of the pressure formed technique (SmileFast™) to rehabilitate a patient presenting with functional and aesthetic problems of multifactorial aetiology:
Pressure formed technique used to restore ten maxillary anterior and premolar teeth with direct composite


A female patient was diagnosed with fractured anterior teeth; erosive, attritional and abrasive tooth wear, and failed existing restorations including a loose fixed/fixed bridge (UR345).

A pre-operative scan of the patient’s teeth was used to manufacture a digital ‘wax-up’. This was then used to make a translucent silicone template (SmileFast™), to simplify restoration of all of the maxillary anterior and premolar teeth using direct composite in a single appointment. The ‘wax-up’ was designed so that the restorations had adequate composite thickness to resist functional occlusal stresses.1,2


Minimally invasive veneer preparations (UR12 & UL12345) preserved the maximum amount of enamel, which was etched with phosphoric acid before adhesive application and light curing.

Composite, heated to 60°, was injected into the silicone template (highly filled flowable composites may also be used). The innovative lab-made template was constructed with detachable, thin metal, interdental separators to reduce the risk of the composite restorations sticking together on insertion. Care was taken to ensure that sufficient composite was injected to allow slight excess. The translucent matrix enabled visual access to check for air bubbles/voids. It also allowed light curing from all angles and minimised the oxygen inhibited surface layer of unpolymerised composite resin. NB: alternative techniques include chairside construction of the template using a translucent silicone material e.g. Memosil (Kulzer) and progressive insertion to allow restoration of individual teeth one at a time.2

Perforations in the accurately fitting template minimised the amount of composite excess. Following template removal, the restorations were light cured again, and the retained interdental separators were removed from between the teeth.

Accurately copying the diagnostic ‘wax-up’ dramatically reduced the finishing and polishing stage.

The completed composite veneers were assessed to ensure that they conformed to the pre-operative functional and aesthetic prescription.
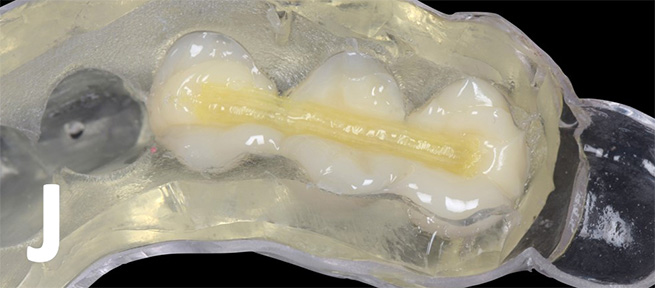

Following removal of the failed bridge (UR345), a printed model was made from a digital impression of the abutment teeth, which had been re-prepared to maximise retention and resistance form. The model was used with the SmileFast™ template to construct a three-unit fibre-reinforced composite resin-bonded bridge at chairside. The strengthening composite fibres were orientated longitudinally in the unset composite resin before insertion onto the model and light curing through the template.

The fibre-reinforced composite bridge retainers and pontic were refined with rotary instruments and the restoration was tried into the patient’s mouth to assess the marginal fit and ensure that its contour conformed to the pre-existing occlusal scheme.

The bridge was then cemented onto the isolated and primed abutment teeth using dual-cure composite resin luting cement.

The patient was reviewed two weeks post-operatively to allow for any occlusal and/or aesthetic adjustments, to check periodontal health, and to reinforce oral hygiene, maintenance and monitoring instructions. When using direct composite, protective mouthguards are usually unnecessary.2

The final image shows the minimally invasive composite restorations two-years postoperatively and demonstrates successful functional and aesthetic integration with the patient’s natural dentition and soft tissues.
References
Dietschi D, Saratti CM. Interceptive treatment of tooth wear: a revised protocol for the full moulding technique. International Journal of Esthetic Dentistry. 2020;15(3):264-286.
Parmar D. Minimally invasive direct restoration of worn teeth: a simplified technique. Dental Update 2019; 46: 388–395

Ahmed Samer Tadfi
BDS BSc(Hons)
GDP (Harrow & Fulham), StyleItaliano Silver member (2021)
